The first preferred diagnostic method for the diagnosis of dermoid cysts is naturally ultrasonography (USG) because it is within easy reach, and is easy to use. The ideal method, to which the ultrasonographic diagnostic criteria—I will list a little later—can be applied, is vaginal ultrasonography. I could not find any article about abdominal ultrasonography, i.e. any article that contains the comparison of vaginal and abdominal USG. But since dermoid cysts contain sebaceous material, it can be confused and cannot be detected if a bowel cleaning is not done properly (1).
Basically, the most important point in the diagnosis is the the doctor’s suspicion. Therefore, he/she must definitely examine the patient, and if there is a mass in the ovary area, i.e. adnexial area, that can be felt bimanually, a better review should be made by means of ultrasonography.
It is because, even if the control is made vaginally, sometimes the sebaceous material that it contains is confused with the fat content of the bowels; o mature cystic teratomas could be overlooked; or an evaluation could be made by considering the existence of a cysts when, in fact, there is no cysts. In a study published from Turkey, 147 of 155 cases diagnosed with dermoid cyst were found to be real dermoid cyst cases during the surgery (2). In the study, the sensitivity (ability to identify sensitive, i.e ill individuals) was found to be 94%. This rate is a little bit optimistic.
On the other hand, the sensitivity for the detection of dermoid cyst in the study carried out by Mais et al. was 84.6% (3).
“Dermoid protrusion” is what is typically observed in vaginal ultrasonography. In fact, if it needs to be completely identified, the complex mass composed of sebum and hair with a certain fat–fluid level is observed. This protrusion-shaped mass observed in the dermoid cyst is called “Rokitansky Nodule” (2,3). This protrusion can be observed in a typical dermoid cyst; however, it may disappear if the fat ratio is high between fat-fluid images, which sometimes seem to be leveled.
In the figure below, you see the USG (ultrasonography) output of a 16-year-old girl. The basic rule is that masses filled with fluid are seen black on USG images (we call it hypoechogen). You can see the “Rokitansky nodule” at the lower part of the cyst.
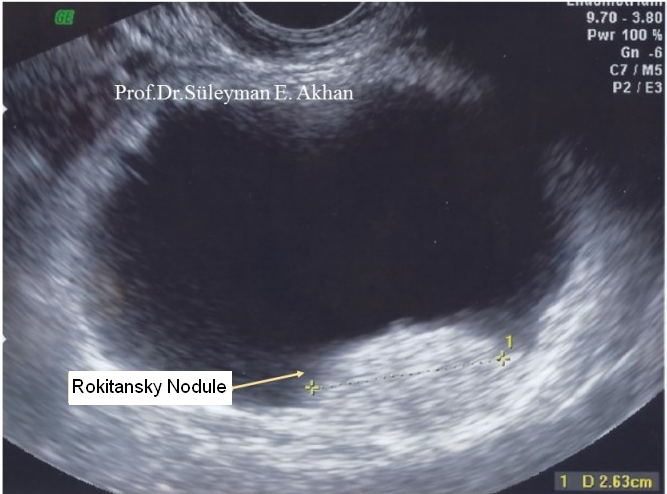
“Rokitansky nodule” on the rectal USG image of the 16-year-old girl
Uyarı: +18 Doğrulama Gerekmektedir.
Görüntülemeye çalıştığınız içerik/görsel +18 doğrulama gerektirmektedir.
Eğer 18 yaş ve üzeri olduğunuzu doğruluyorsanız "e-posta" sekmesine
e-posta adresinizi yazarak, "Doğrula" butonuna tıklayınız.
Even in the studies conducted 20 years ago, the sensitivity of MRI in the diagnosis of dermoid cyst was found to be 100% (4).
I believe it is required to have a MRI test before surgery of a patient diagnosed with dermoid cyst. I listed the reasons below, in my own way. But for all these reasons that I listed in an academic context, it is questionable but at the point that I reached alfter years, I believe that any patient should not be taken into operation without having a “Contrast-enhanced fat-suppressed MRI”. I have listed my reasons below.
Reasons that Necessitate a Preoperative MRI:
- Diagnosing the mass as a dermoid cyst (mature cystic teratoma) with an accuracy close to 100%. (There is always a margin of error)
- Understanding if there is a dermoid cyst in the other ovary, for being able to talk to the patient and her family. It is because any unneeded interventions will affect the patient’s fertility. The probability of detecting a dermoid cyst in the other ovary is 12% to15% (Literature). Therefore, knowing whether there is a cyst in the other ovary before the surgery would prevent unnecessary incisions on the relevant ovary or prevent the surgeon from overlooking the existing cyst.
- There may be malignant tumor in dermoid cysts, at the rate of 0.2% to 2%. These tumors have often a “squamous” cells structure. Both the actual size of the cyst and excessive grown squamous cell tumor—even if not always available—can be observed on MRI. It can cause the surgeon to get suspicious and do the operation accordingly.
- Since mature cystic teratomas (Dermoid Cysts) inherently originate from the 3 germ layers that constitute the embryo, they contain hair, sebum, sebaceous material, and sometimes bone and teeth. These bones may belong to any part of the body. The problem is that when the bone structure in the content of the dermoid cyst is big, it would be difficult to strip the cyst and preserve the ovary during the laparoscopic surgery. Therefore, I think it is better to prefer open surgery to remove dermoid cysts that contain a big bone structure. MR gives clear information about this issue, as well.
What you see below is the bone structures of a 18-year-old patient with 20 cm dermoid cyst, and the fat-liquid level in that cyst.
[/optinlocker]
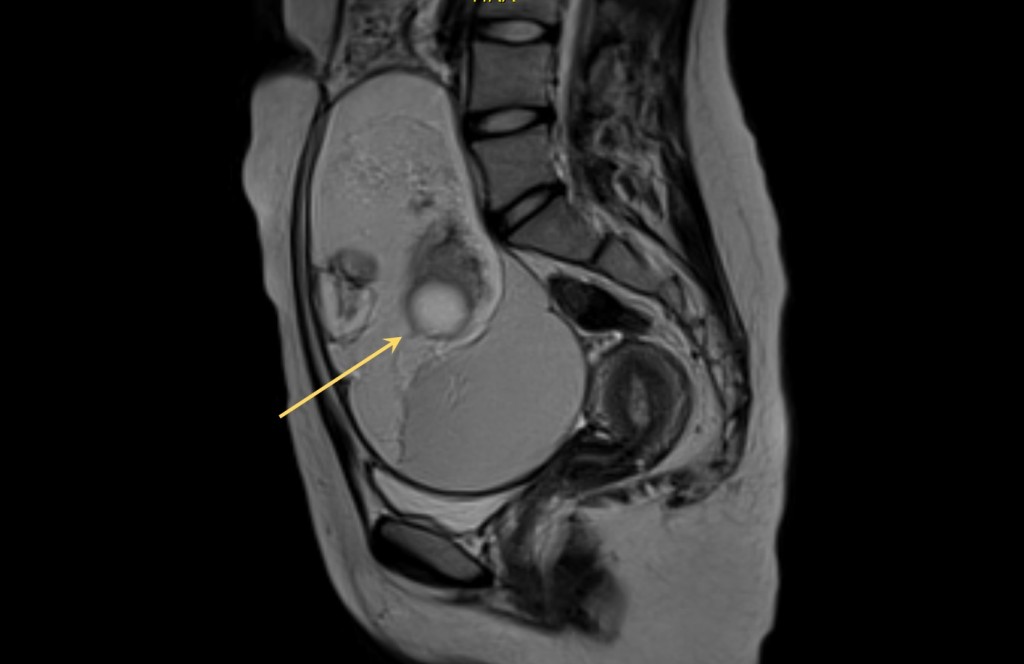
MR images of 20 cm dermoid cyst in a 18-year-old girl.
References
1. http://emedicine.medscape.com/article/281850-workup#c4
2. Ekici E, Soysal M, Kara S, Dogan M, Gokmen O. The efficiency of ultrasonography in the diagnosis of dermoid cysts. Zentralbl Gynakol. 1996;118(3):136-141.
3. Mais V, Guerriero S, Ajossa S, Angiolucci M, Paoletti AM, Melis GB. Transvaginal ultrasonography in the diagnosis of cystic teratoma. Obstet Gynecol. 1995; 85: 48-52
4. Scoutt LM, McCarthy SM, Lange R, Bourque A, Schwartz PE. MR evaluation of clinically suspected adnexal masses. J Comput Assist Tomogr. 1994; 18(4):609-618.
5. Coskun A, Kiran G, Ozdemir O. CA 19-9 can be a useful tumor marker in ovarian dermoid cysts. Clin Exp Obstet Gynecol. 2008;35(2):137-139.
